

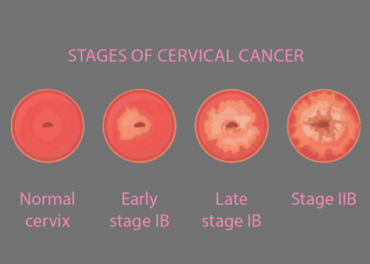
Pap smears, visual inspection with acetic acid (VIA), and visual inspection with Lugol's iodine (VILI) are all methods for screening cervical cancer:
• Pap smear: The USPSTF recommends that women aged 21–29 get their first Pap test at age 21, and then get a Pap test every three years.
• VIA: A visual examination of the cervix after applying acetic acid.
• VILI: A visual examination of the cervix after applying Lugol's iodine. Lugol's iodine reacts with glycogen, which is present in precancerous lesions and cancer, causing them to turn yellow.
The World Health Organization (WHO) recommends that women who test positive for HPV undergo VIA/VILI screening.
The diagnostic accuracy of VIA and VILI varies across studies. For example, VIA sensitivity ranges from 55% to 96%, and specificity ranges from 49% to 98%.
Introduction. Cancers of the female reproductive tract, referred to as gynecological cancers, are diagnosed in nearly 1.4 million worldwide and lead to 15% of all female cancer deaths [1]. The three most common gynecological malignancies are cervical, endometrial (uterine), and ovarian
Assessment
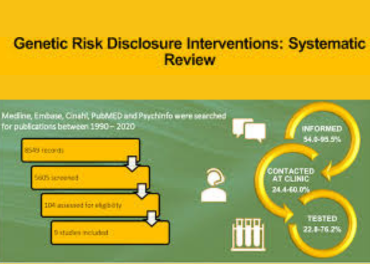
A medical professional evaluates your personal and family history, including pathology and imaging reports, to assess your risk for hereditary cancer.
Genetic testing
A blood or saliva sample is sent to a lab for analysis to check for harmful gene variants that may be present in your family. There are several types of genetic tests available, including panel tests that look for variants in multiple genes at once.
Counseling
Before and after genetic testing, a medical professional can help you understand the results, discuss other cancer risks, and identify educational needs.
If you test positive for a hereditary cancer gene mutation, your medical provider may recommend risk reduction interventions, such as surgery to remove healthy ovaries and fallopian tubes.
Some other ways to reduce your risk of cancer include:
• Living smoke-free
• Being sun safe
• Maintaining a healthy body weight
• Eating well
• Moving more and sitting less
• Limiting alcohol

There are many types of biopsies, including excisional and core needle biopsies, which can be performed in an outpatient clinical setting:
Biopsy type
Description
Excisional biopsy
The entire tumor or suspicious area is removed, along with some normal tissue around it. This procedure is also known as an open biopsy.
Incisional biopsy
Only a portion of the tumor is removed.
Core needle biopsy:
A sample of the mass is removed, which can be used to establish a pathological diagnosis.
The type of biopsy that's performed depends on the location of the tissue or fluid being examined, and whether a more destructive or malignant lesion is suspected. For example, an excisional biopsy is usually preferred when melanoma is suspected.
Other types of biopsies include:
• Bone marrow biopsy
• Cone biopsy
• Liquid biopsy
• Punch biopsy
• Sentinel node biopsy
• Shave biopsy
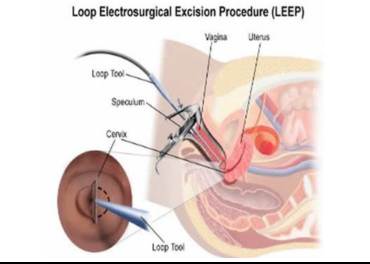
Colposcopy is a noninvasive procedure where a device similar to a microscope magnifies your cervix to make abnormal growth easier to see. LEEP is used to diagnose and treat cervical dysplasia and conditions like genital warts and polyps.
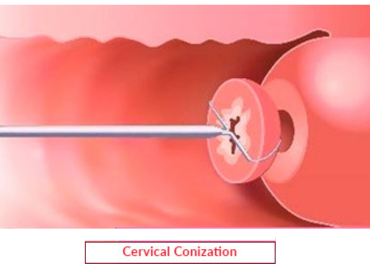
During a cone biopsy, surgeons cut a larger, cone-shaped section of abnormal tissue from your cervix using a surgical knife. Cone biopsy is a more complicated surgery, and surgeons perform it under general anesthesia. The recovery time is longer, and it carries more risk than LEEP.
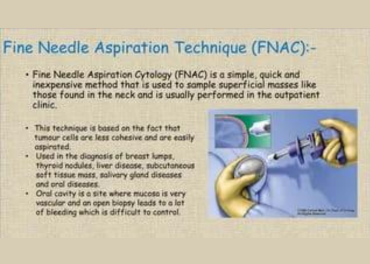
FNA, indeed, is the investigation of choice for the detection of a suspicious lesion at superficial sites. FNAC is the first line of investigation to evaluate abdominal wall masses and can help in the definitive diagnosis, thus avoiding unnecessary surgical intervention in the majority of cases.
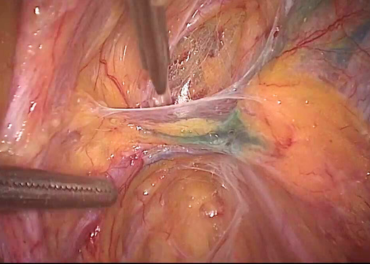
In rare cases, a suspected ovarian cancer may be biopsied during a laparoscopy procedure or with a needle placed directly into the tumor through the skin of the abdomen. Usually the needle will be guided by either ultrasound or CT scan.

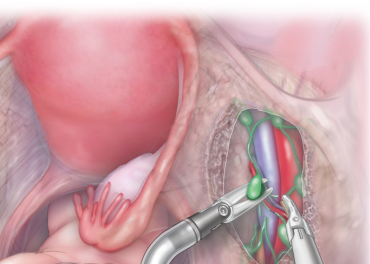
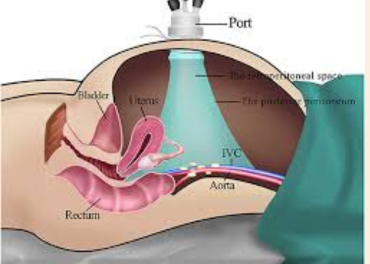
Laparoscopic hysterectomy and pelvic lymphadenectomy is a minimally invasive surgical procedure that can be used to treat early-stage endometrial cancer. It can be a safe and effective alternative to the open surgical approach, with the following advantages:
• Shorter operative time
• Less blood loss
• Less pain
• Less scarring
• Shorter hospital stay
• Faster recovery time
Some other benefits of laparoscopic hysterectomy and pelvic lymphadenectomy include: Avoiding abdominal incision wound infection and Reduced risk of vaginal recurrence.
However, this procedure should only be performed by oncologic surgeons who are trained in extensive laparoscopic procedures.
Some complications of these surgeries include: nerve or vessel damage, excessive bleeding, wound infection, blood clots, and damage to nearby tissues.
Primary cytoreductive surgery (PCS) and interval cytoreductive surgery (ICS) are two different surgical strategies for treating advanced ovarian cancer. Both approaches can lead to better survival outcomes if they achieve complete cytoreduction, or minimal residual disease.
Laparoscopic staging for endometrial cancer is generally considered a safe and feasible alternative to laparotomy, and has several advantages, including:
Fewer complications
Laparoscopic staging is associated with lower rates of postoperative complications, such as wound infection, blood loss, and bowel obstruction.
Shorter hospital stay
Laparoscopic staging is associated with shorter hospital stays than laparotomy.
Less pain and bleeding
Laparoscopic staging is associated with less pain and bleeding than laparotomy.
Faster recovery
Laparoscopic staging is associated with faster recovery to normal activities than laparotomy.
However, some issues remain to be resolved, such as:
Standardization
There are still some conflicting ideas about the staging system, and the first aim should be to standardize what is needed for staging.
Randomized studies
Randomized studies are still needed to standardize the indications and applications of laparoscopic pelvic and paraaortic lymphadenectomy.
Robotic-assisted laparoscopy
While early reports suggest that robotic-assisted laparoscopy is feasible, the number of patients in these reports is small, and they lack control or comparison groups.

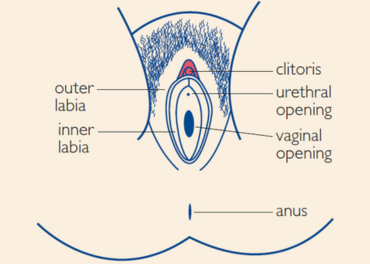
A skinning vulvectomy is a type of vulvectomy surgery that removes only the top layer of skin affected by cancer, while a radical vulvectomy removes the entire vulva and deep tissues. A radical vulvectomy with groin node dissection is a surgical procedure that removes the vulva and lymph nodes in the groin area.
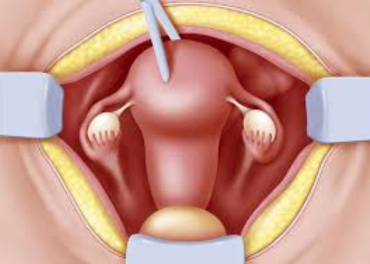
A radical hysterectomy is a type of surgery that removes the uterus and may also remove the ovaries, fallopian tubes, and nearby lymph nodes. It can be performed using an open technique, which involves making a large incision in the abdomen. The incision can be either low transverse, just above the pubic area, or vertical, between the navel and the pubic area.

Robotic assistance can be used in pelvic exenteration surgery, a complex procedure that involves removing the pelvic organs:
Advantages
Robotic assistance can provide better views of the pelvis, increased dexterity, and a greater range of motion. This can be helpful in operating in the pelvis's confined spaces.
Considerations
Robotic surgery can be expensive, as it requires purchasing the robot and disposable instruments. The cost can also vary depending on the surgeon's experience and the procedure's requirements. The robotic arms may also conflict with each other if they aren't placed far enough apart. This can be a problem for patients with a small abdomen or low BMI.
Outcomes
Minimally invasive surgery techniques can be used for certain patients with favorable tumor characteristics and anatomy. Studies have shown good perioperative outcomes for these patients.
Pelvic exenteration is a major surgery with a significant rate of complications. Patients and providers should be prepared for a long and potentially complicated hospital course.
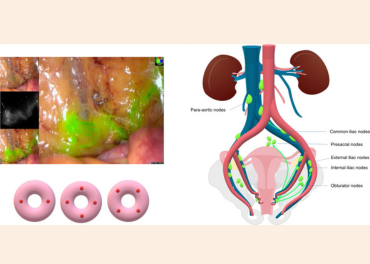
A sentinel node biopsy (SLNB) is a procedure that can be used to diagnose and stage vulvar and endometrial cancer:
Vulvar cancer
SLNB is recommended for the management of vulvar cancer. It can detect small amounts of cancer that aren't visible on scans or felt as swelling.
Endometrial cancer
SLNB is the preferred technique for nodal staging of low- and intermediate-risk endometrial cancer. It can provide prognostic information and reduce the morbidities associated with full lymphadenectomy (LND).
Here's how a SLNB works:
1. A radioactive substance or blue dye is injected near the tumor.
2. The injected material is located using a device that detects radioactivity or visually.
3. The sentinel node, which is the first lymph node to take up the material, is removed and checked for cancer cells.
If the SLNB is positive, the sentinel node will have shown metastases in either the standard histopathological assessment or ultrastaging. If both tests are negative, the sentinel node is considered negative.
If the SLNB fails, a side-specific lymphadenectomy may be required, along with removal of any suspicious lymph nodes.

Hyperthermic (or Heated) Intraperitoneal Chemotherapy (HIPEC) is a surgical procedure that's giving new hope to patients with abdominal cancers. Immediately after removing visible tumors through what's called cytoreductive surgery, our surgeons pump a powerful dose of heated chemotherapy inside a patient's abdomen.
Omentectomy, pelvic and paraaortic lymphadenectomy, and peritonectomy are all surgical procedures that are sometimes performed in gynecologic oncology:
Omentectomy
Removes part or all of the omentum, a fatty layer that covers the abdominal organs. It can be performed to treat or prevent ovarian cancer, or to reduce the risk of cancer spreading to other organs. There are different types of omentectomies, including total and partial.
Pelvic and paraaortic lymphadenectomy
A common surgical procedure in gynecologic oncology. Paraaortic lymph node dissection is a challenging retroperitoneal surgery that helps with staging, prognosis, and surgical management.
Peritonectomy
Removes diseased peritoneum, the serous membrane that surrounds the stomach and other abdominal organs. There are different types of peritonectomies, including complete and selective parietal peritonectomy.